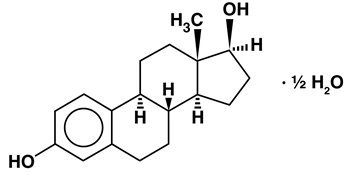
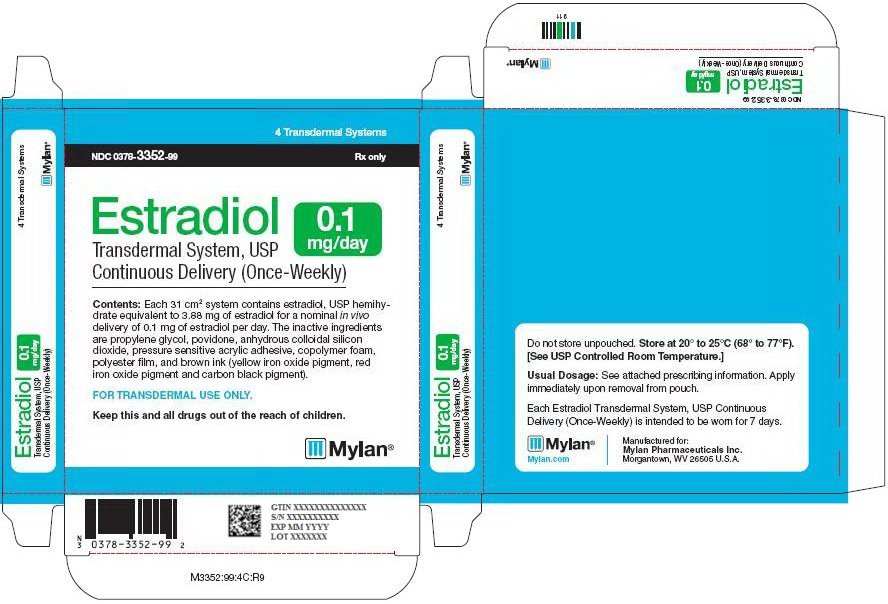
Have been on vivelle dot patch for more years. Or PA who is well-versed in bio-identical hormone replacement therapy. And have tried to wean off several. Estradiol Patch official prescribing information for healthcare professionals. Includes: indications, dosage, adverse reactions, pharmacology and more.
Anyone know how to come in for an easy landing with an HRT patch? I am sick of the swollen boobs and bloating, I get some hot flashes anyway, so I took the patch off last Saturday. All was well at first. Boobs went down and no more cramps or bloating.
Last night, it hit the fan! I got hot over mother's house, had to take off my coat a few times, sweating under the arms and then got the chills a few minutes later. Last night I had night sweats. Woke up 2 x and had to change nightgown. I was soaked!
My neck was soaking wet, under the arms, and from the waist up. I make my room cold and it was just a disgusting feeling waking up all wet in a freezing room. Dropped the nightgown to the floor put on a clean one (I have them all lined up) and went back to bed. Few hours later? HAPPENS AGAIN! So this morning I put the patch back on! When does this end?
A small number of women find the patch form of estrogen delivers too high a dose, dumping in body fat. These women prefer to take transdermal estrogen where they can control dosage at low levels.
I want to get off this patch! I worry about using this HRT stuff but haven't had success with anything else in the least.
For postmenopausal women who discontinue hormone therapy (HT), tapering treatment appears overwhelmingly favored over a sharp halt, researchers found. A survey of more than 480 physicians in two large integrated health groups in the Northeastern and Northwestern U.S. Found that 91% of respondents advised tapering when discontinuing oral HT, compared with just 8% who advocated immediate cessation.
The primary method - cited by 60% of physicians surveyed - was to decrease both the dose and days per week of HT, Katherine M. Newton, PhD, of the Group Health Research Institute in Seattle, and colleagues reported in the July/August issue of Menopause. Discontinuation became a big issue in the wake of the Women's Health Initiative (WHI) study results published in 2002 showing with use of hormone replacement therapy. Rates of postmenopausal hormone usage dropped by roughly half for estrogen plus progestin while estrogen-only use fell by more than a quarter during the first year after publication of the WHI results, Newton's group noted. Today, discontinuation remains an issue; most guidelines recommend that if HT is going to be used, it be used primarily to treat vasomotor symptoms at the lowest possible dose and for the shortest possible duration. However, there are no guidelines or randomized trial data to address best practices for how to stop HT, Newton and colleagues explained. They surveyed physicians within two large integrated healthcare systems - Harvard Vanguard in the Northeast and Group Health in the Northwest U.S.
with questionnaires sent between December 2005 and May 2006. The analysis included reports from 483 eligible physicians (78.5% response rate), excluding nonphysician respondents and those who never prescribe or counsel patients on hormone therapy. Among the respondents, 432 were family practitioners or internists while 60 were Ob/Gyn practitioners.
Practice type appeared to influence attitudes toward discontinuation. Family physicians or internists were more aggressive about encouraging women to stop hormone therapy as soon as possible, scoring an average of 2.2 compared with the Ob/Gyn average of 2.9 on a five point scale in which a score of 5 was 'let women use hormone therapy as long as they want.' Female physicians, too, were 90% more likely than their male counterparts to encourage women to discontinue as soon as possible (27% versus 17%), which was a significant difference even after adjustment for site and physician type. The physicians in the Northeast were also more likely than those in the Northwest to recommend discontinuation. Stopping the use of hormonal patches was trickier.
Almost 60% of physicians reported no experience with tapering patches. Those who did taper HT patches said they mostly increased the days between applying the patches, though a sizable proportion had cut patches into smaller sizes. The authors did not gather information on hormonal creams and gels.
Estrogen Patch Reviews
In figuring out how to discontinue these drugs, the biggest influence was the physician's own experience (48%), followed by advice from colleagues (25%), and the woman's preference (19%) - whereas research evidence was cited by only 2% of survey respondents. Systemic estrogen therapy is the only therapy approved by the FDA for treating hot flashes. According to the North American Menopause Society, there is a 50% chance that hot flashes and other symptoms will recur after HT is stopped. To manage hot flashes after discontinuing HT, most physicians endorsed behavioral changes (44%) and increased exercise (37%), as well as phytoestrogens from black cohosh (28%) or eating more soy (26%) despite evidence suggesting no benefit from these alternative therapies.
Ob/Gyn practitioners advocated drug therapies more often for managing return of symptoms compared with primary care physicians:. Resume hormone therapy (43% versus 15%). Start gabapentin (Gabarone, Neurontin, 7% versus 1%). Start clonidine (Catapres, 12% versus 5%) Again, female physicians were more likely to recommend nonhormonal therapies to deal with symptoms after adjustment for practice type. Overall, these results highlighted the lack of standard protocols to deal with discontinuation and 'a need to create an evidence-based approach to hormone therapy discontinuation,' Newton's group wrote in the paper. They cautioned about generalizing these health-plan specific findings to larger regions but noted that the results supported national statistics.